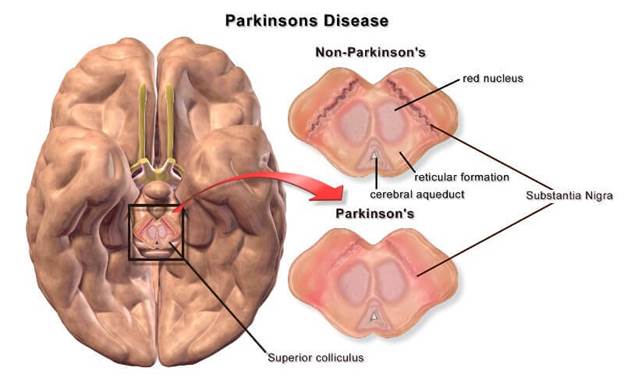
Parkinson’s disease is a progressive neurological disorder that primarily affects movement. It occurs due to the gradual loss of dopamine-producing neurons in the brain, leading to symptoms like tremors, rigidity, and bradykinesia (slowness of movement). Over time, non-motor symptoms such as depression, sleep disturbances, and cognitive decline can also emerge. Traditionally, Parkinson’s has been managed rather than cured, making advancements in treatment crucial for improving quality of life for patients.
Traditional Approaches to Parkinson’s Treatment
For many years, treatment centered on medications like Levodopa, which replenishes dopamine levels in the brain. Other drugs, including dopamine agonists and MAO-B inhibitors, were often added to manage symptoms and extend the effectiveness of Levodopa. Physical therapy was also recommended to maintain mobility. While these methods improved motor symptoms, they often led to side effects such as dyskinesia and did not address non-motor complications effectively.
The Role of Advanced Medications and Drug Therapies
In the past decade, medication strategies have advanced significantly. Extended-release formulations of Levodopa now provide more stable symptom control, reducing fluctuations experienced by patients. Additionally, newer drugs targeting both motor and non-motor symptoms have entered clinical practice. These include COMT inhibitors, which enhance Levodopa’s effect, and medications designed to manage depression and cognitive impairment associated with Parkinson’s disease.
Deep Brain Stimulation: A Game-Changer in Treatment
Deep Brain Stimulation (DBS) has become a transformative surgical option for patients who do not respond well to medications. This technique involves implanting electrodes in specific brain areas to regulate abnormal neural activity. Recent improvements include directional leads and rechargeable batteries, allowing better symptom control with fewer complications. DBS is now considered earlier in the treatment timeline for eligible patients, offering greater flexibility in managing advanced Parkinson’s.
The Emergence of Non-Motor Symptom Management
Earlier approaches to Parkinson’s often focused exclusively on motor issues, but research has highlighted the importance of non-motor symptoms such as anxiety, constipation, and cognitive decline. Treatments now incorporate psychiatric medications, gut health interventions, and cognitive therapy. This shift acknowledges that comprehensive care must address both physical and mental well-being for optimal patient outcomes.
Rehabilitation and Lifestyle Interventions for Better Outcomes
Lifestyle modifications and rehabilitation therapies have gained prominence. Physical therapy continues to be important, but new emphasis is placed on speech therapy, occupational therapy, and specialized exercise programs such as dance or boxing for Parkinson’s. These interventions improve motor control, speech clarity, and overall quality of life, reducing the risk of falls and complications.
Technology in Parkinson’s Care Like Wearables and Apps
Technology has revolutionized patient monitoring. Wearable devices track tremors, gait, and medication adherence, providing real-time data for physicians. Mobile apps now assist patients in logging symptoms, scheduling medications, and accessing teleconsultations. These tools enable personalized treatment plans, early detection of changes, and more efficient doctor-patient communication, ensuring better disease management even in remote areas.
Stem Cell Research and Future Prospects
Stem cell therapy represents one of the most promising areas of research in Parkinson’s treatment. Scientists aim to replace damaged dopamine-producing neurons with healthy ones derived from stem cells. Although still in clinical trial stages, this approach could potentially restore motor function and slow disease progression. Other research directions include gene therapy and disease-modifying drugs designed to target the underlying causes of Parkinson’s.
Access to comprehensive Parkinson’s care often depends on geography. Cities with advanced medical infrastructure offer patients specialized neurologists, advanced therapies, and modern research participation. Ahmedabad, for example, has emerged as a hub for neurological care with its well-equipped hospitals and highly trained specialists. Patients seeking holistic treatment approaches can benefit from this infrastructure through services like Parkinson’s Disease Treatment in Ahmedabad, where multi-disciplinary teams work together to ensure personalized care using the latest advancements.
What the Next Decade Could Hold for Parkinson’s Treatment
Looking ahead, treatment strategies are likely to become more personalized, with therapies tailored to a patient’s genetic profile and disease progression. Advances in neuroimaging and artificial intelligence will enhance early detection, while wearable technology will integrate seamlessly into routine care. Combined with advancements in regenerative medicine, the next decade could change Parkinson’s management into a more proactive and targeted approach.
read more : Are AI Employees the Next Step in Workforce Automation?