Primary liver cancer, most commonly hepatocellular carcinoma (HCC), remains a major global health burden, especially among high-risk populations with underlying chronic liver disease. With increasing incidence rates in the United States—more than 41,000 new cases estimated in 2024 alone according to the American Cancer Society—the need for early detection and effective management is urgent.
While traditional risk factors such as hepatitis B and C infections, alcohol use, and cirrhosis are well documented, advancements in molecular biology have brought genetic and molecular markers into the spotlight. These factors not only enhance our understanding of hepatocarcinogenesis but also pave the way for precision medicine.
Explore the various types of liver cancer and their molecular underpinnings to enhance diagnostic precision and personalise treatment strategies.
The Landscape of Primary Liver Cancer
Hepatocellular carcinoma accounts for approximately 75% to 85% of primary liver cancer cases, while intrahepatic cholangiocarcinoma (ICC) and other rare forms make up the remainder. Molecular characterisation is increasingly critical in distinguishing these subtypes, as they exhibit different biological behaviours and therapeutic responses.
Understanding the molecular heterogeneity of these tumours is crucial for implementing personalised oncology care, particularly given that liver cancer often presents late, when curative options are limited.
Genetic and Molecular Risk Factors: An Overview
1. TP53 Mutations
The TP53 tumour suppressor gene is one of the most frequently mutated genes in HCC. These mutations are associated with poor prognosis, aggressive tumour phenotype, and resistance to chemotherapy. According to data compiled by The Cancer Genome Atlas (TCGA), TP53 mutations occur in roughly 30%–50 % of HCC cases, particularly in non-cirrhotic livers and those related to aflatoxin B1 exposure.
Clinical relevance: TP53 mutations may help predict patient response to immune checkpoint inhibitors and serve as a potential biomarker for clinical trials.
2. CTNNB1 (Beta-Catenin) Mutations
CTNNB1 mutations, affecting the Wnt/β-catenin pathway, are detected in about 20% – 40% of HCC cases, especially in tumours without significant inflammatory infiltration. These mutations are often linked to well-differentiated tumours and better prognosis, but are also associated with immune exclusion, potentially reducing response to immunotherapy.
Clinical relevance: The Wnt/β-catenin pathway is a potential target for therapeutic intervention, and CTNNB1 mutation status may inform treatment selection.
3. TERT Promoter Mutations
Telomerase reverse transcriptase (TERT) promoter mutations are among the earliest genetic alterations in hepatocarcinogenesis. Present in more than 60% of HCC cases, these mutations upregulate telomerase activity, enabling cellular immortality and malignant transformation.
According to the National Cancer Institute (NCI), these mutations are commonly found in cirrhotic livers, implicating them as an early biomarker for malignant transformation.
Clinical relevance: Screening for TERT promoter mutations could support early diagnosis and identify patients at high risk for progression from cirrhosis to cancer.
4. AXIN1 and ARID1A
Mutations in tumour suppressor genes such as AXIN1 and ARID1A play a role in chromatin remodelling and Wnt signalling. Although these mutations are less frequent (approximately 10%–15% of cases), they are associated with worse survival outcomes and more aggressive disease phenotypes.
Clinical relevance: While not yet actionable targets, these mutations provide insight into tumour biology and may guide future research directions.
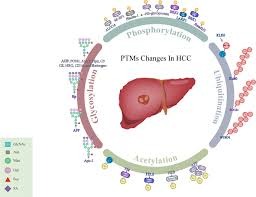
Epigenetic Alterations and Non-Coding RNAs
Beyond genetic mutations, epigenetic modifications—such as DNA methylation and histone acetylation—are involved in liver tumorigenesis. Aberrant methylation of tumour suppressor genes (e.g., RASSF1A, GSTP1) has been observed in both early and advanced HCC.
Additionally, non-coding RNAs, especially microRNAs (miRNAs), serve as promising diagnostic and prognostic biomarkers. For example, miR-122, highly expressed in normal liver tissue, is often downregulated in HCC and associated with poor prognosis. The NIH highlights ongoing clinical trials exploring miRNA-based diagnostics and therapies.
Clinical relevance: Liquid biopsy-based detection of epigenetic markers and miRNAs could offer non-invasive diagnostic tools for early detection and disease monitoring.
Molecular Subtypes of HCC
Modern transcriptomic profiling has classified HCC into distinct molecular subclasses, each with unique clinical implications:
- Proliferation class: Characterised by high AFP levels, chromosomal instability, and activation of proliferation pathways like IGF, MET, and mTOR.
- Non-proliferation class: More indolent, with frequent CTNNB1 mutations and better prognosis.
The proliferative class is typically associated with HBV infection, poor differentiation, and higher risk of metastasis, while the non-proliferative class is more commonly linked to HCV and alcohol-related liver disease.
Clinical relevance: This subclassification provides a framework for predicting treatment response and designing biomarker-driven clinical trials.
Hereditary Syndromes and Genetic Susceptibility
Although most cases of primary liver cancer are sporadic, hereditary conditions can increase susceptibility. Notable examples include:
- Hereditary Hemochromatosis (HFE mutations): Chronic iron overload promotes oxidative stress and liver fibrosis, leading to a 20- to 200-fold increased risk of HCC.
- Alpha-1 Antitrypsin Deficiency (SERPINA1 mutations): Misfolded protein accumulation causes hepatocyte injury and cirrhosis, predisposing patients to HCC.
Clinical relevance: Genetic testing for at-risk individuals can guide early surveillance strategies and inform family counselling.
Integrating Molecular Markers into Clinical Practice
As molecular profiling becomes more accessible, integrating these markers into clinical workflows can significantly improve outcomes. Several key uses include:
- Risk Stratification: Genetic and molecular markers help identify high-risk patients for enhanced screening and surveillance protocols.
- Therapeutic Decision-Making: Targeted therapies, such as tyrosine kinase inhibitors (e.g., sorafenib, lenvatinib) and immune checkpoint inhibitors (e.g., nivolumab, atezolizumab/bevacizumab), are more effective when selected based on underlying molecular features.
- Monitoring and Prognosis: Tracking molecular markers over time can aid in assessing treatment response and detecting recurrence.
Conclusion
Primary liver cancer, especially HCC, is no longer a monolithic disease. With growing insight into molecular and genetic factors, we now understand it as a collection of diverse subtypes driven by unique biological mechanisms. From TERT promoter mutations and TP53 abnormalities to miRNA deregulation and epigenetic shifts, these markers not only elucidate the pathways of carcinogenesis but also offer tangible benefits for diagnosis, treatment, and prognosis.
Healthcare professionals are encouraged to stay informed on emerging data and incorporate molecular insights into clinical decision-making. As more targeted therapies and diagnostic tools become available, precision oncology in liver cancer is moving from theory to standard practice, offering hope for better outcomes in this challenging disease.
READ MORE : Battery Storage: The Key to Sustainable Energy Resilience