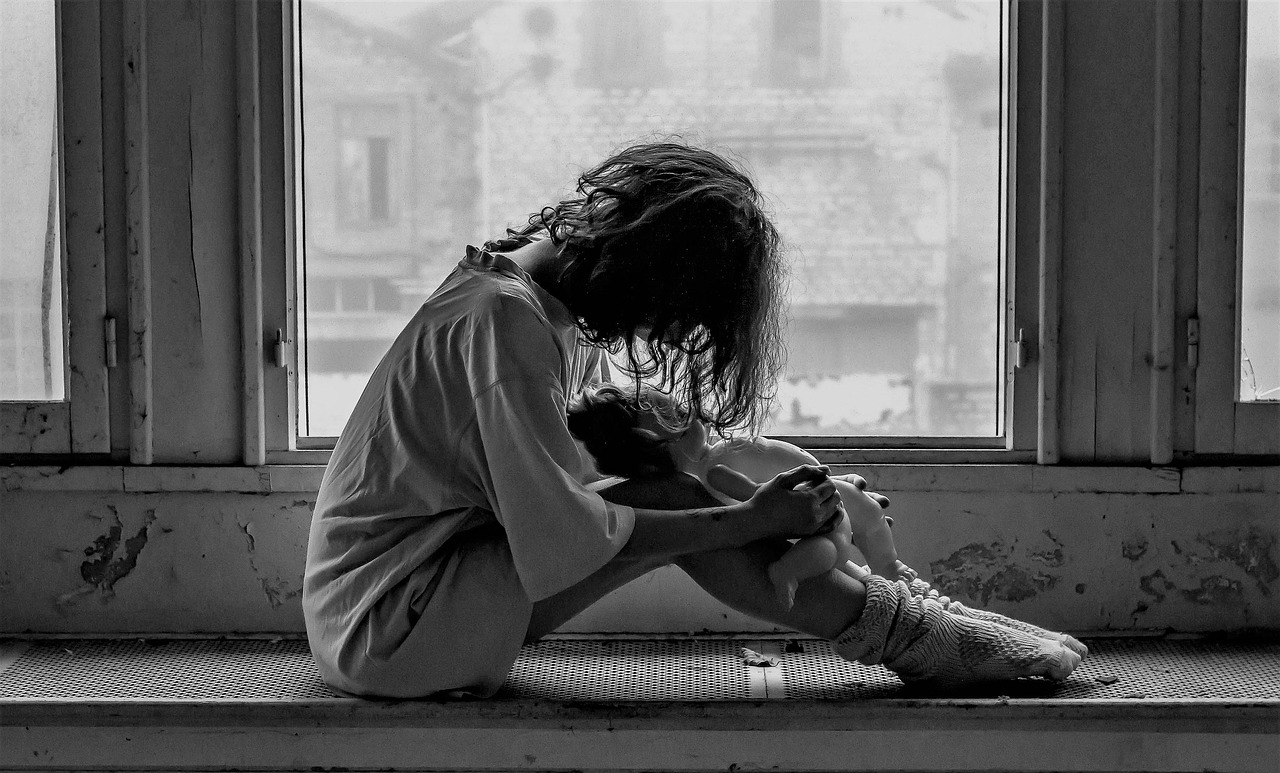
Muscle Tension and Chronic Pain Feed into Negative Emotions
When you’re tight—perhaps in your neck, shoulders, jaw—you’re sending pain messages to your brain constantly. That raises your baseline stress. Over time, that low-grade pain runs mood down, feeds anxiety, and amplifies irritability.
You notice the pain more and recover less. Sleep is affected. Your resilience wanes. Mental health interventions need to work with that tension, not around it.
Poor Posture and Body Misalignment Affect Energy and Mood
Sagged or slouching posture pushes your chest down, constricts breathing, and demobilizes core muscles. You lose energy in the long run. You get tired. You also get into a feedback loop: when you’re low, you slouch more—this perpetuates negative body messages to your brain.
Correcting posture alters body feedback. You’re more present. You’re more here. That is good for your emotional state.
Body Awareness Builds a Bridge to Internal States
Too often, you lose touch with what your body is actually doing. You may not even be aware when you tense up muscles or when you hold your breath. Without awareness, you can’t let go. You must learn to feel into your body—where it’s tightening up, where it’s hurting—in order to have a chance to intervene sooner, before the pain gets ahead of you.
That consciousness gives you “early warning signs” of emotional stress or relapse risk. You can then attend to the body before the mind crashes.
Body Care within Behavioral Health
You need more than a mental health plan—you need a body-mind plan. Following are some key areas to include:
Posture Work and Movement Habits
Integrate simple posture checks into your daily life. Head over shoulders, up straight, relax knees. Try movement breaks—roll shoulders, open chest. Work on breaking static position.
Within the treatment space, therapists and counselors can integrate movement reminders or short body scans. You need to move and re-set.
Pain Management and Manual Therapies
If you live with chronic pain, get help. Physical therapists, chiropractors, massage therapists, myofascial release or trigger-point therapy can ease tension hotspots. Less pain over time equals less emotional load.
This doesn’t lessen your mental health work. It complements it. The less your brain is encumbered by pain messages, the more energy it has to put into healing mood, cognition, and coping abilities.
Body Awareness, Breath, and Somatic Techniques
Body scan exercises, diaphragmatic breathing, progressive muscle relaxation—all aid in mapping areas of tension. Body scanning brings underground tension to the level of awareness. You then let go of tension.
Teaching you to stop, breathe, notice the body is equipping you to jump into action when tension is about to escalate. You no longer accept total breakdowns.
Coordinated Care: Behavioral and Physical Experts Working Together
Behavioral healthcare professionals must collaborate with physiotherapists, pain specialists, movement coaches. That makes your treatment integrative. The physical professional prescribes posture and pain release; the mental health professional monitors mood, stress, triggers.
If you’re in residential or outpatient treatment, look for centers that treat dual needs. For example, a Florida Mental Health Treatment Center that includes physical care in its programming can offer a more holistic recovery path.
Likewise, if you have both drug addiction or alcoholism and mental illness, go to a dual-diagnosis program that addresses your whole body. A treatment facility that is seasoned at treating Dual Diagnosis in Washington might include physical care in the program.
How Body Care Contributes to Stability of Mood, Lower Relapse
Reduced Stress Reactivity
Pain and tension work like constant alarms. The more you lower them, the more your baseline of physiological stress goes down. Your system will cope better with emotional triggers when you face them. You’re less likely to feel in control.
Better Sleep, Better Recovery
Simpler to sleep with less pain. Good posture adds to alignment and comfort. Sleep helps with mood regulation, memory storage, and emotional resilience.
Gain in Self-Efficacy
When you actively work on your body—by stretching, breathing, posture exercise—you regain a sense of control. You’re no longer a passive patient, but an active partner. That empowerment is what keeps you following your recovery plan.
Preventing Physical Stress from Causing Relapse
Untreated tension or pain can trigger relapse. You may use maladaptive coping or substances to suppress the pain. But if you have systems to release body stress ahead of time, you short-circuit that cycle: body stress → emotional distress → relapse.
Steps You Can Take Today
- Build a posture check moment every hour.
- Try a 5-minute body scan or progressive muscle relaxation.
- Get guidance from a physical therapist or massage therapist in releasing tension.
- Talk over your body goals with your behavioral health provider—ask for coordination.
- Monitor your daily levels of tension and pain so you catch rising trends.
Conclusion
Healing from behavioral health works when the body and mind are healed together. Care for your body—relieving tension, strengthening posture, cultivating body awareness—improves mood, reduces stress, and reduces the likelihood of relapse. If you want to achieve sustained recovery, you must connect your body to your treatment plan.
Your healing is your work. Don’t leave your body behind.
also read: How to Choose the Right Docking Station for Dual Monitors?